Dysbiosis: the missing link
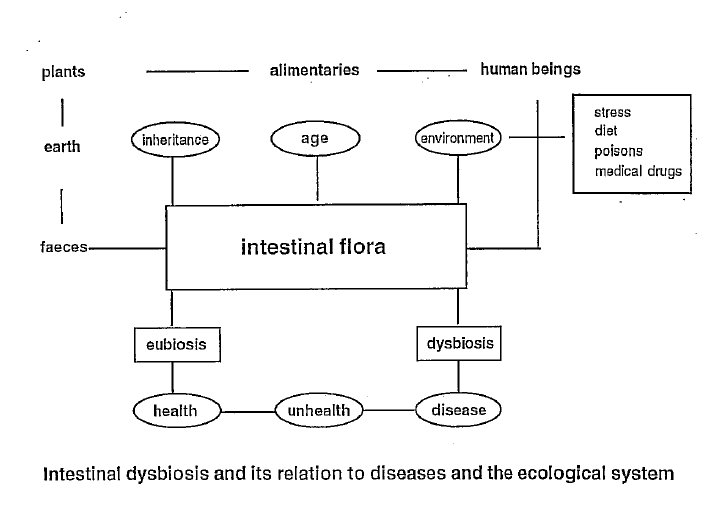
This booklet will give information about intestinal dysbiosis. This condition is characterised by an imbalanced intestinal bacterial flora. It will explain the relationships between food and lifestyle and its impact on health and diseases. In the intestine, micro-organisms influence our body functions in many different aspects, i.e., biochemically and immunologically. It is most important to treat the microflora in an enlightened probiotic direction.
These probiotics, often some sort of lactic acid producing cultures, are able together with the host’s own flora, to deal with disturbances due to inadequate food, stress and strain, environmental toxins and different medical drugs such as antibiotics, contraceptives, painkillers etc.
The intestinal flora influence the immune system and regulate the body’s ability to cleanse itself of waste products, i.e., detoxification. A harmonised and balanced flora will contribute to a better absorption of nutrients, i.e., minerals, trace elements, vitamins and amino acids.
Intestinal Dysbiosis
What is dysbiosis?
Dys- means faulty and -bios is life and growth. This implies faulty life. In biological terms, the phrase intestinal dysbiosis is used for an unbalanced bacterial flora in the intestine. You could say the microflora is dysbiotic. Normally, it is understood this condition includes harmful metabolic activity of the flora.
How does dysbiosis develop?
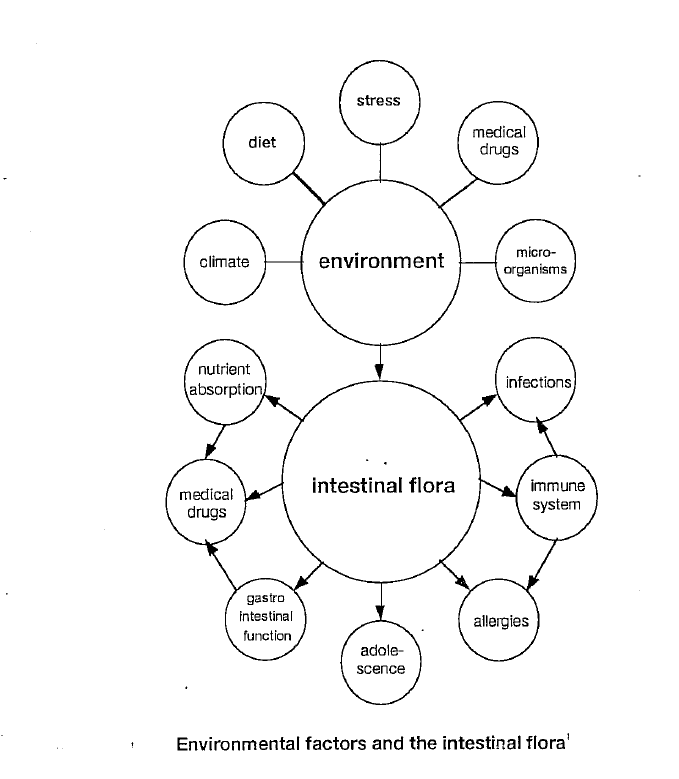
There are many factors that influence what type of bacteria or micro-organisms will grow or colonise in the gastrointestinal channel. In the mouth, there are already quite a number of bacteria. Many of them come from the intake of food. In the ventricle, the amount will be reduced. In the small intestine, the numbers of bacterial cells increase from the beginning towards the end (i.e., E5 to E9–10/g content). You’ll find the highest amount of bacteria in the colon (i.e., E10–11/g content). Stress, food, medical drugs, environmental toxic loading, and climate are all factors that stimulate or inhibit different types of micro-organisms. A poorly balanced diet will create a dysbiosis.
Different life situations with psychic stress or disharmony are also very influential in creating a dysbiosis. A great number of medical drugs inhibit the beneficial flora from acting normally. Environmental toxins can also provoke an intestinal dysbiosis. Food supplements taken inadequately will disturb the important balance. It should be noted that the climate supports a variety of different bacterial cultures. This is often experienced when travelling, i.e., tourist diarrhoea.
What conditions or diseases depend on dysbiosis?
Dysbiosis will often show as functional disturbances in the ventricle or the intestine. Symptoms such as dyspepsia, constipation or loose stools are conditions that will later develop into gastritis and chronic inflammation in the intestine. Ulcers in the ventricle or the intestine could result if the dysbiosis is not properly regulated. Gallbladder problems and obstipation or diarrhoea are often related to intestinal dysbiosis. Dysbiosis can also manifest in dysfunction of the immune system, i.e., food intolerance. Atopies or allergies, i.e., eczema and urticaria, are of similar origin. Chronic inflammatory diseases, i.e., arthritis, are also developed in the context of dysbiosis. Certain types of migraine, where food and diet are significant in the outbreak, could be a symptom of intestinal dysbiosis.
How will dysbiosis be inhibited?
Through the stimulation of beneficial bacteria in the intestine, the degree of dysbiosis will be reduced. Optimising the food intake and avoiding detrimental stress, mental and physical welfare can be disrupted by harmful medical drugs, environmental toxins and micro-organisms. There are not many of us that can live in total harmony. This would be an utopia. To be successful in this, you must learn what is beneficial and what is harmful for the intestinal flora in general and in each case.
Eubiosis and Probiosis
What is probiotics?
Lactic acid bacterial cultures, so-called probiotics, stimulate colonization of the so-called human autochthonous flora in a beneficial direction. Probios means for life. A condition without any dysbiosis is called eubiosis. It is more likely to be an utopia. Reducing the degree of dysbiosis is called probiosis. That is why the cultures are called probiotics.
As a therapist, you of course advise your patient to optimise all the factors mentioned above. A well-balanced diet and life pattern is the best insurance for being healthy. In most cases, probiotics could be an important, if not crucial, complement.
Bifidobacterias and Bacteroides
What bacteria are there in the stomach and the intestine?
When fasting, you only find small quantities in the stomach. Together with the intake of food, the amount of bacteria will increase to E5 cfu/ml liquid. There often are streptococci, bifidobacteria, enterobacteria and bacteroides—some of them emanating from the mouth and the food itself. These will be reduced when the stomach starts producing acid and the pH is reduced. Further down in the small intestine, the number of cells increases again; E5–7 cfu/ml content.
In the colon, the numbers increase dramatically. The two dominating types of cultures are bacteroides and bifidobacteria. There are about E10–11 cfu/g faeces. The weight is 0.5–1 kg! The total amount is E14. This is related to the total amount of human body cells, which is E13. This implies there are 10-fold more micro-organisms than body cells! This is of great importance, especially when referring to the immune system. The Peyer’s patches in the small intestine play the most important role in the control and balance of the immune system and its relation to the microflora. There is a microeco-intesto-immuno-endocrino-neuro-psycho linkage.
This explains many of the syndromes described, where you find both physical and psychiatric disorders closely related to each other.
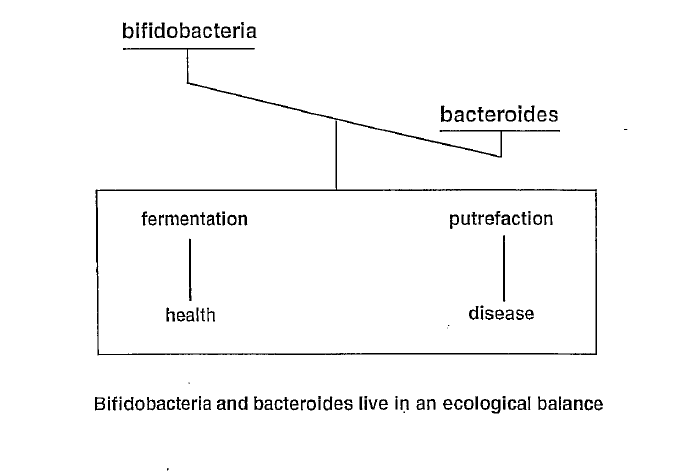
Fermentation and Putrefaction
Simplified, you could separate the bifidobacteria as the good ones and the bacteroides as the evil ones. Bifidobacteria split the food by fermentation. Lactic acid, acetic acid and butyric acid are produced. These will create a more acidic environment in the intestine.
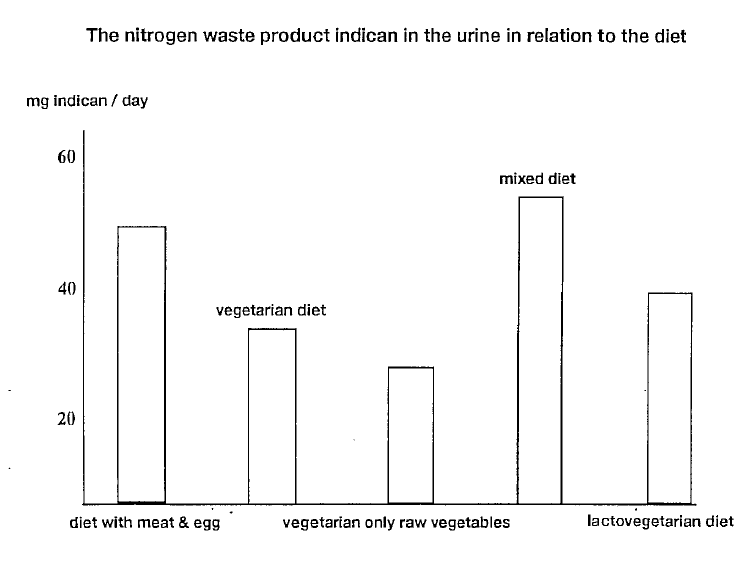
The bacteroides will digest the food by putrefaction. It will then produce nitrogen waste products. These are harmful for the human body, and they will be absorbed in the intestine, reaching all the different body tissues.
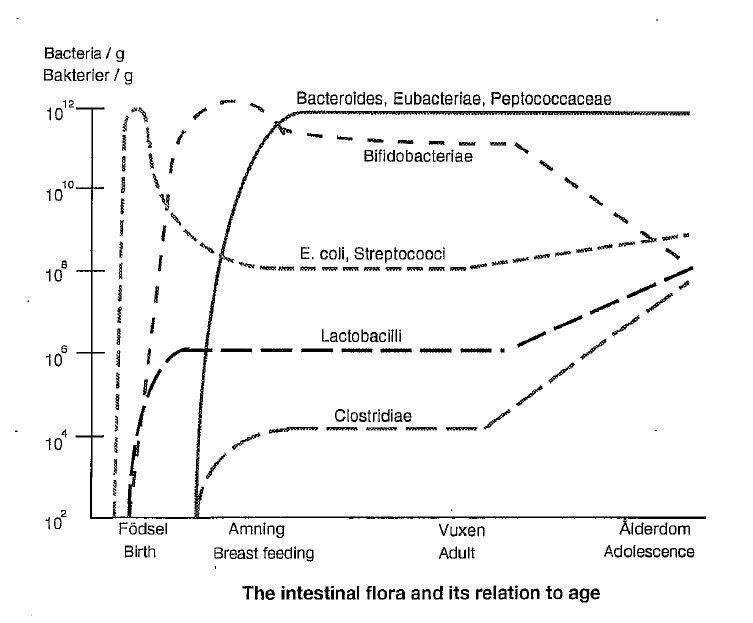
Streptococci, enterococci, and enterobacteria (i.e., colibacteria) are found in minor quantities. In adolescents, the quantity of bifidobacteria is lower.
This is shown on page nine.
What sort of diet promotes a healthy flora?
Food rich in complex carbohydrates with a low glycemic index. These are broken down relatively slowly and will provide you with a steady blood sugar level. Vegetables of different types, rice, and pasta are adequate roughage.
A high intake of protein and animal saturated fatty acids stimulates the activity of bacteroides towards putrefaction. In western society, we strain our bodies with the intake of too much protein and saturated fatty acids. The WHO standard protein requirement is approximately 0.8 g/day/kg body weight.
An intake of high amounts of fibre improves the motility of the intestine. This promotes the bifidobacteria. A vegetarian diet contains many different food fibres such as cellulose, hemicellulose, and pectin. An intake of fibres should always be followed by intake of water.
The term “throw water” is adequate. It indicates enough hydration.
The Immune System and Lymphoid Tissue
The intestinal flora communicate with the immune system through the so-called lymphoid tissue. This tissue is found in crypts in the small intestinal mucosa. It is called the Peyer’s plaque. Deeper in the intestinal tissue there is the lamina propria with lymphoid tissue. All this is connected together with lymphatic vessels directed towards the lymph nodes. These are located in the mesenteric fibrous tissue that lines the small intestine. This is related to the other parts of the immune system. The intestinal-related immune system is in this manner able to read and translate or react on the biochemical activities in the intestine.
The immune system is stimulated or inhibited by different bacterial cultures or food items. Dysbiosis creates a disharmony in this complicated relationship. The human being is born with a genetic memory that decides what sort of food will be accepted or not. If we introduce new unknown food items into the body, there is a risk that the immune system will react against them.
Certain probiotics can induce an immunogen effect. It means B- and T-lymphocytes are stimulated and the concentration of immunoglobulins is increased. Probiotics are transitory. They do not normally colonise on the intestinal mucosa.
Nitrogen Waste Products
What happens in the intestine biochemically and immunologically during probiotic therapy?
Those enzymes the body itself uses for digesting food are influenced directly or indirectly by all the micro-organisms there are in the stomach and the intestine. This is called enzyme induction. Certain compounds that are produced in the digestion of food are toxic and cause harm in different tissues. When there is intestinal dysbiosis, these compounds are found in high quantities.
Probiotics will reduce the dysbiosis and thereby the accumulation of toxic waste products. When protein is digested through the action of these harmful intestinal micro-organisms, directly or indirectly, a variety of nitrogen waste products—such as ammonia, urea, indols, phenols, nitrites, and nitrosamines—will be produced.
These toxic items could, in a later sequence, influence the outcome of different unhealthy conditions, i.e., chronic diseases where the immune system is seriously involved. They also promote the development of polyarthritis and skin diseases.
Normally, the liver is able to detoxify all these toxins. However, if the load is heavy and prolonged, the liver will not be able to cleanse completely.
Detoxification and Retoxification
Certain beneficial bacteria are able to neutralise toxic metabolites. This is called detoxification. The opposite is retoxification. It is the conversion of non-harmful products to harmful ones. Probiotics reduce the pH in the intestine, causing the activity of the coliform putrefactive bacteria, such as bacteroides and clostridia, to be inhibited. The production of their metabolites will then be reduced. Additionally, the absorption of these is impaired, resulting in them being excreted in the faeces.
Conjugation and Deconjugation
One of the methods the liver uses to neutralise toxins is by conjugating them with glucuronic acid, thereby creating glucuronides. This process is called conjugation. When these are excreted from the gallbladder out into the intestine, it is given the capability to get rid of toxins.
When there is a dysbiotic condition in the intestine, certain bacteria improve their ability to digest these conjugates. This is called deconjugation. The toxins are reabsorbed into the blood. The result is retoxification.
Some of the enzymes that deconjugate and retoxify toxic waste products are:
- Beta-glucuronidase
- Azoreductase
- Nitroreductase
The outcome of their action is an increased accumulation of toxic metabolites. By probiosis, this will be reduced.
Glycosides from different green plants, such as rutin, may be converted by the action of Streptococcus faecium to quercetin. This molecule is mutagenous. It will cause injuries to the body cell’s genetic code. This can develop into malignant conditions, i.e., cancer.
Streptococcus faecalis is responsible for another sort of retoxification. It converts the amino acid tyrosine to tyrosamine. An increased amount of tyrosamine is thought to trigger attacks of migraine. In a later phase, this amine is converted to phenol, which is mutagenous.
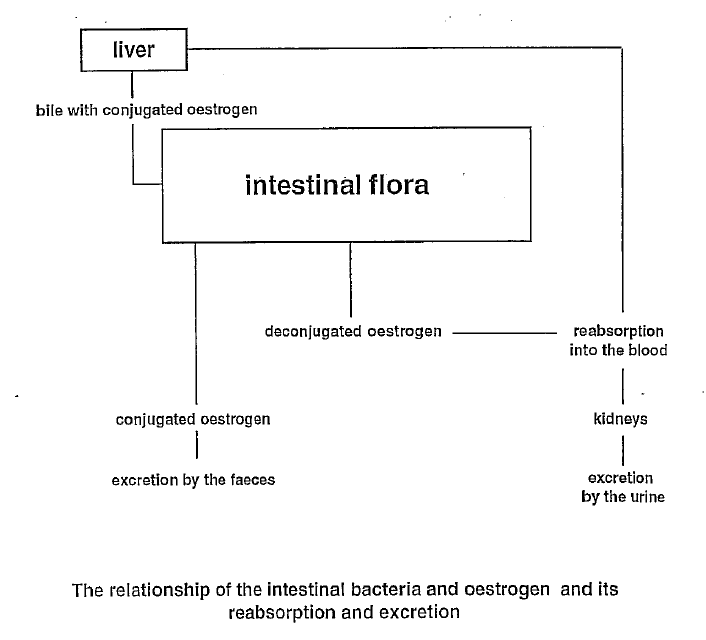
Oestrogen
Bile acids, cholesterol, and a variety of sex hormones are exposed by the same mechanisms, i.e., conjugation and deconjugation. They are excreted by the bile into the intestine. Further down in the intestinal channel, they are reabsorbed. A certain amount is lost in the faeces. A loss of volatile bile acids and, to a certain degree, cholesterol are lost in the same manner, which could be favourable.
It is not desirable for the sex hormones to be lost in the faeces. Both female and male hormones can be lost in this manner. This happens when there is an intestinal dysbiosis. A reduced concentration of oestrogen can cause:
- Bleeding disturbances
- Increased sensitivity to genital infections (i.e., vaginitis)
- Bladder infections (i.e., cystitis)
- Impaired fertility
- Osteoporosis with pain syndrome
You may experience similar mechanisms when taking contraceptives and antibiotics at the same time.
Endotoxins
When there is dysbiosis, certain bacteria (i.e., clostridia) produce endotoxins, which will influence the immune system. A great number of chronic inflammatory diseases are related to dysbiosis. These immune-related diseases will appear in various soft tissues such as the skin, joints, urinary system, intestine, eyes, glands, etc.
Carcinogens and Insulin
Deconjugated bile acids and cholesterol are to be converted further in a later phase. The harmful bacteria stimulate the production of an increased amount of volatile secondary bile acids and coprostanol, which is a digested product of cholesterol. These are carcinogenic, including the above-mentioned enzymes and the nitrosamines. They promote the initiation of different types of cancer, e.g., breast cancer.
An unbalanced intake of short and rapidly digested carbohydrates (i.e., glucose) intensifies the development of dysbiosis. Note the glycaemic index of different food items and their bioavailability.
There is an insulin-like substance produced by E. coli bacteria. It is a sort of analogue. This substance is thought to be absorbed into the blood and situate itself on the receptors where human insulin is normally positioned. Thereby, it will inhibit the action of insulin.
In diabetic patients, you often find dysbiotic conditions.
Vitamins and Analogues
The bacterial flora in the colon produce a variety of vitamins. The absorption of these is relatively poor. It is impossible to estimate how important this vitamin production is. All of the B vitamins and the K vitamin are produced. The latter is essential for coagulation ability. Most of our need is absorbed in the small intestine.
What is of more interest is that bacteria consume vitamins for their own survival. When there is dysbiosis, this consumption is increased in the lower part of the small intestine. Vitamin B12 will in this manner be consumed. Depressed levels of vitamin B12 are seen amongst older people; compare this with the reduced action of the bifidobacteria.
It is known that bacteria are able to produce so-called vitamin analogues. These analogues compete with the real vitamins. They act as ghosts and are believed to cause functional conditions of insufficiency. The traditional tests on vitamin B12 are inadequate and insufficient. The level of homocystein gives a better understanding of the vitamin condition. It could also in some cases function as an indirect parameter estimating dysbiosis.
As mentioned above, the autochthonous flora create a barrier and protection against hostile and not welcoming guests. The majority of the pathogen or disease-provoking bacteria are sensitive to competition from the natural flora.
When there is dysbiosis, their establishment will be facilitated. Probiotics reduce the pH in the intestine by 1–2 units. This will aggravate the establishment of, e.g., salmonella, cholera, etc.
The bifidobacteria defend their territory by producing different organic acids, i.e., acetic acid, lactic acid, and special natural antibiotics.
Certain Conditions When Probiotics Are of Importance
Below is a variety of conditions more or less related to intestinal dysbiosis.
The dysbiotic condition is directly or indirectly related to symptoms.
- Gastritis and ulcer
- Gallbladder dysfunction and liver diseases
- Constipation or irritable colon
- Obstipation or diarrhoea
- Dyspepsia
- Migraine; conversion of tyrosine to tyrosamine
- Atopies (e.g., eczema, hay fever, urticaria, asthma)
- Food intolerance (e.g., gluten intolerance)
- Chronic inflammatory or autoimmune diseases (e.g., rheumatism, SLE, fibromyalgia, psoriasis, colitis ulcerosa, Crohn’s disease)
- Infections in the urinary system
- Mycosis (e.g., Candida albicans)
- Exposure to radiation, cortisone, antibiotics, contraceptives
- Conditions with impaired immune defence (e.g., malignant diseases such as leukaemias)
- Insufficiency of vitamins or minerals
- Stress
- Skin diseases (e.g., acne, herpes)
- Hormonal dysfunction (e.g., bleedings, menstruation dysfunction, infertility, osteoporosis)
- Metabolic syndrome and diabetes
- Chronic fatigue syndrome
These conditions illustrate when probiotics may be particularly beneficial, due to their potential role in restoring balance to the intestinal flora.
Leave a Reply